Help Your Dopamine System Help You
– BY LEIF PETERSON, LPC, NCC
Addiction is a complex issue that can manifest in various forms, including substance abuse, gambling, gaming, overeating, compulsive internet, or social media scrolling and others. Later in this blog I will write about my personal story of addiction and how my dopamine system was affected. First, I’ll lay out the scope of the problem and explain how the dopamine system plays a part. Here are some general statistics on addiction:
- Substance Abuse:
- According to the National Survey on Drug Use and Health (NSDUH) in the United States, approximately 20.4 million adults had a substance use disorder in 2019.
- Opioid addiction is a significant concern, with over 2 million Americans suffering from opioid use disorder (OUD) in 2018, according to the National Institute on Drug Abuse (NIDA).
- Alcohol addiction is prevalent globally. The World Health Organization (WHO) reports that harmful use of alcohol results in approximately 3 million deaths each year.
- Smoking:
- Tobacco addiction remains a global health challenge. The WHO estimates that there are over 1 billion smokers worldwide, with tobacco-related illnesses causing around 8 million deaths annually.
- Gambling Addiction:
- The prevalence of gambling addiction varies by country and region. In the United States, it’s estimated that around 2-3% of the population has a gambling problem, according to the National Council on Problem Gambling.
- Internet and Gaming Addiction:
- Internet and gaming addiction are relatively newer concerns. The prevalence rates vary widely across studies, but some suggest that around 1-10% of gamers may experience significant gaming-related problems. Some form of internet-related problems are prevalent in my clientele.
- Effects on Mental Health:
- Addiction often co-occurs with mental health disorders. For example, individuals with substance use disorders are more likely to have mood disorders like depression or anxiety.
- Addiction can also have severe social and economic consequences, including strained relationships, financial problems, and legal issues.
- Treatment and Recovery:
- Despite the challenges, effective treatments are available for addiction. These can include therapy, medication, support groups like Alcoholics Anonymous (AA) or Narcotics Anonymous (NA), Recovery Dharma and SMART Recovery, and lifestyle changes.
- Recovery from addiction is possible with appropriate support and resources. However, it often requires long-term management and commitment.

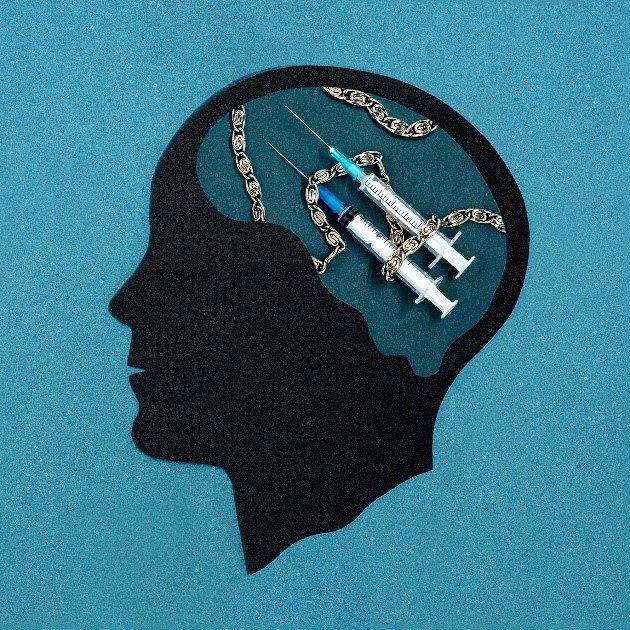
How does dopamine reinforce addiction?
The feeling of pleasure is how a healthy brain identifies and reinforces beneficial behaviors, such as eating, socializing, and sex. Our brains are wired to increase the odds that we will repeat pleasurable activities. The neurotransmitter dopamine is central to this. Whenever the reward circuit is activated by a healthy, pleasurable experience, a burst of dopamine signals that something important is happening that needs to be remembered. This dopamine signal causes changes in neural connectivity that make it easier to repeat the activity again and again without thinking about it, leading to the formation of habits.
Just as drugs produce intense euphoria, they also produce much larger surges of dopamine, powerfully reinforcing the connection between consumption of the drug, the resulting pleasure, and all the external cues linked to the experience. Large surges of dopamine “teach” the brain to seek drugs and other addictive behavior at the expense of other, healthier goals and activities.
Cues in a person’s daily routine or environment that have become linked with drug use because of changes to the reward circuit can trigger uncontrollable cravings whenever the person is exposed to these cues, even if the drug itself is not available. This learned “reflex” can last a long time, even in people who haven’t used drugs in many years. For example, people who have been drug free for a decade can experience cravings when returning to an old neighborhood or house where they used drugs, or smell something like cigarette smoke which can be linked to nicotine addiction or another addictive behavior to which smoking was linked. Like riding a bike, the brain remembers.
Why are drugs more addictive than natural rewards?
For the brain, the difference between normal rewards and drug rewards can be likened to the difference between someone whispering into your ear and someone shouting into a microphone. Just as we turn down the volume on a radio that is too loud, the brain of someone who misuses drugs adjusts by producing fewer neurotransmitters naturally in the reward circuit, or by reducing the number of receptors that can receive signals. As a result, the person’s ability to experience pleasure from naturally rewarding (i.e., reinforcing) activities is also reduced.
This is why a person who misuses drugs eventually feels flat, without motivation, lifeless, and/or depressed, and is unable to enjoy things that were previously pleasurable. Now, the person needs to keep taking drugs to experience even a normal level of reward—which only makes the problem worse, like a vicious cycle. Also, the person will often need to take larger amounts of the drug to produce the familiar high—an effect known as tolerance.
I Know How It Feels to Have a Disordered Dopamine System
After becoming paralyzed from a fall right before my 18th birthday, I was given opioids to cope with the substantial pain associated with that injury. I can still remember one of the first times I was given a shot of a powerful opioid when I was lying in a hospital bed, unable to move my body below my chest. I felt devastated by this injury and did not know how I was going to get through it. After receiving that shot of an opioid medication, it changed my mental state instantaneously. I was still paralyzed, I was still laying in that hospital bed not knowing what my life would look like going forward, but with the opioids flooding my brain with dopamine, increasing pleasure and inhibiting stress and anxiety, it suddenly did not feel as devastating. It felt tolerable. It did the job that it was supposed to do at the moment. The problem developed when I kept taking opioid medications for years, and at increasingly higher amounts, to cope with physical and emotional pain caused by living with paralysis. The alcohol, marijuana, nicotine and benzodiazepines added to the problem by flooding my brain with dopamine.
After years of substance use, my brain developed tolerance to the drugs and no longer produced the same euphoric feelings. Tolerance also triggers the brain to increase nerve activity which creates feelings of dysphoria and anxiety. I lost the ability to feel pleasure, motivation or learn important life skills due to addiction to opioids. It became difficult to go through my mail or get outside and get exercise. This is an aspect of addiction it does not seem many people understand: people who struggle with addiction are not solely pursuing more pleasure, they are trying to stop highly unpleasant feelings and just feel normal.
When I tried to stop taking opioids without any medication assistance, my brain and body told me I was going to die if I did not take them. The escalation of my nerves overfiring became so strong that it made my body so rigid that I could not bend my legs at times and spent months in the hospital with chronic spasticity. Not everyone will experience withdrawal symptoms this extreme but are likely to have a range of unpleasant physical and emotional symptoms associated with withdrawal.
It took me years to get off high levels of prescription opioid medication and reprogram my brain to feel pleasurable emotions and sensations without these drugs. Two main tools that worked for me were medication assisted treatment (MAT) and physical exercise. I was given a drug called Buprenorphine to help wean off other opioids. Buprenorphine is a partial opioid agonist that mimics some of the positive effects of stronger opioids, with a longer half-life. This means I did not feel the same level of euphoria from Buprenorphine as I would from stronger opioids, like morphine or fentanyl, but it released enough dopamine to reduce the discomfort from my overactive nerves.
Physical exercise produced a small effect at first by releasing natural endorphins and dopamine. This showed me that I had some control over producing pleasurable feelings naturally, without opioids. The more consistent I became with physical exercise, the stronger and more enduring the effect on my mood. Physical exercise eventually led to other positive effects, like losing weight and making social connections, which triggered my brain to release more dopamine. My dopamine system had healed enough that activities like playing basketball and making friends actually felt good again! This was the beginning of my path back from a disordered, addicted brain, with a depleted dopaminergic system.
Your Path Back from Addiction
First, a note about my approach to addiction counseling: I am not dogmatic in my approach to counseling people struggling with addiction. I have made significant progress on several addictive behaviors including alcohol, nicotine, marijuana and opioids, and your path will inevitably be different than mine. I have helped people reduce or eliminate addictive behaviors, and each of their paths of been different. It is vital to find the path that works for you. I see my role as an addictions counselor is to support you mentally and emotionally and offer possible ways to change. It is up to you to make these changes and figure out your own path. Recovering from addiction can feel like wandering a jungle in which no clear path exists. My personal experience with recovery, and professional experience supporting others, will help to point out some trailheads to try and pitfalls to avoid while navigating this jungle. I will provide support and encouragement when you succeed, and empathy and more encouragement when you experience setbacks. One overall goal of recovery from addiction, emphasized in this article, is resetting your dopamine system to allow your brain the best chance to recover from the disorder of addiction. Below are some ideas for steps that can help.
Reset Your Dopamine System
Resetting or rebalancing your dopamine system is an appealing concept, especially for those feeling the effects of burnout, addiction, or mental health issues like depression. Dysregulation of dopamine pathways can contribute to various psychological conditions. Here are several ways to help rebalance or “reset” your dopamine levels:
- Modify Your Diet:
- Eat dopamine-rich foods: Incorporate foods that are rich in tyrosine, the precursor to dopamine. These include bananas, avocados, beans, seeds, and nuts.
- Balance your nutrition: Ensure a balanced intake of proteins, fats, and carbohydrates, which can influence neurotransmitter synthesis and overall brain health.
- Regular Physical Exercise:
- Exercise increases dopamine release and boosts your mood. Activities like running, cycling, and swimming can particularly help increase dopamine levels.
- Adequate Sleep:
- Sleep is crucial for regulating neurotransmitter function. Ensuring you get enough sleep, typically 7-9 hours per night, can help maintain the balance of dopamine.
- Reduce Stress:
- Chronic stress can deplete dopamine and lead to burnout. Techniques such as mindfulness, meditation, yoga, or deep breathing exercises can reduce stress and help maintain dopamine levels.
- Digital Detox:
- Reducing exposure to digital screens, especially those from smartphones and computers, can help mitigate the instant gratification loop associated with dopamine release. Try setting aside specific times when you refrain from using digital devices.
- Therapeutic Interventions:
- Cognitive Behavioral Therapy (CBT), Motivational Interviewing (MI) and other forms of psychotherapy can help manage behaviors that disrupt dopamine balance, particularly in the context of addiction or mental health disorders.
- Medication:
- In some cases, particularly where psychiatric conditions are involved, medication might be necessary to help regulate dopamine imbalances. This should always be managed by a healthcare professional.
- Avoid Drugs and Alcohol:
- Substances like alcohol, nicotine, and recreational drugs can interfere with the natural balance of dopamine and should be avoided or used moderately.
- Natural Sunlight:
- Exposure to natural sunlight can increase the natural production of serotonin, which can in turn support healthy dopamine levels.
- Engage in New Activities:
- Trying new things can stimulate the brain’s reward system, prompting dopamine release. This could involve learning a new skill, hobby, or simply exploring new environments.
Implementing these strategies may help balance your dopamine levels and contribute to better mental and physical health. If you’re trying to reset your dopamine due to a specific health condition, such as depression or addiction, it’s important to consult with healthcare professionals for tailored advice. Recovery from addiction and a disordered dopamine system can be an arduous journey. Try to remember that your brain will heal if you give it the proper nutrition, tools, and time.